News
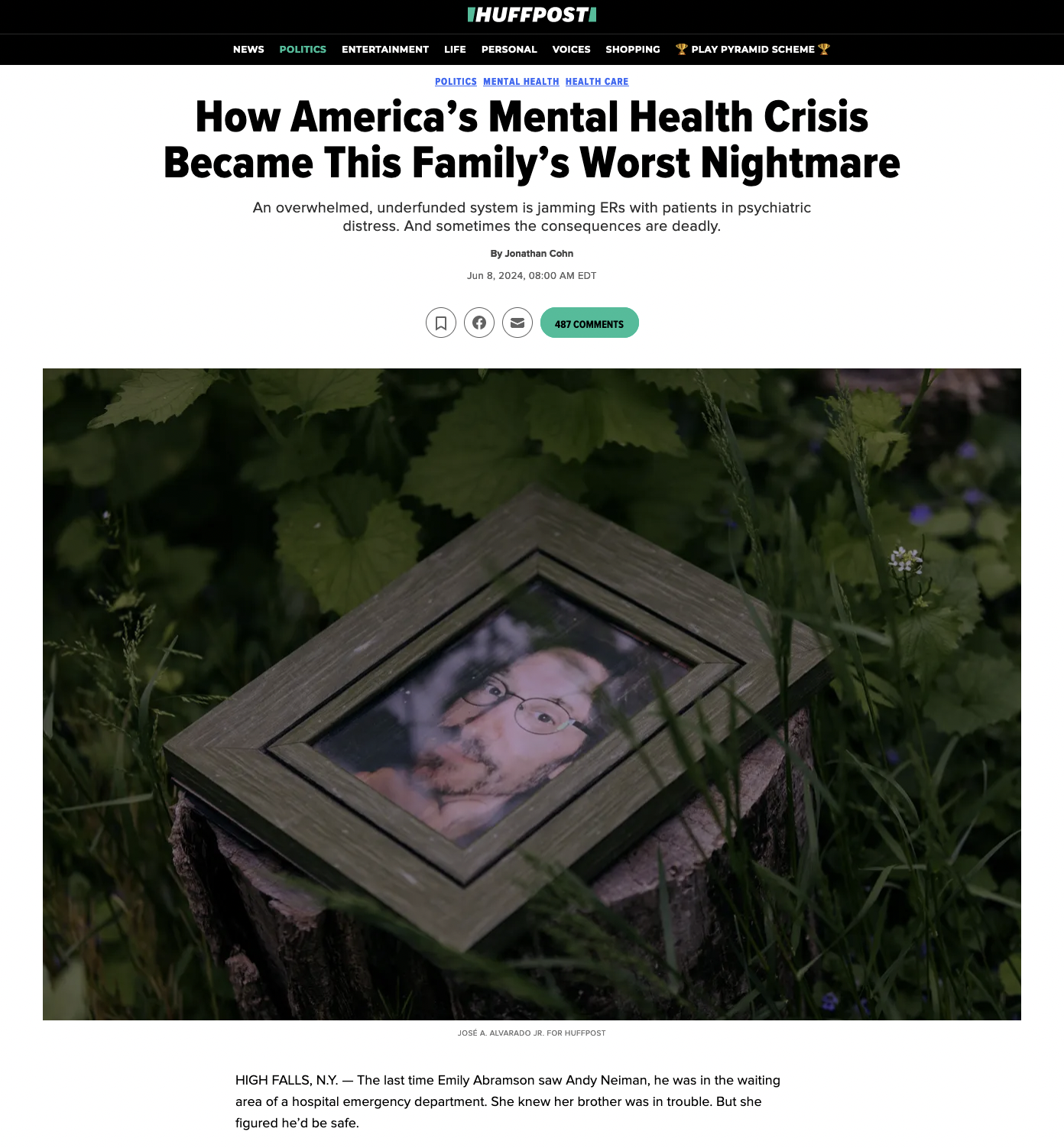
for Huff Post: How America’s Mental Health Crisis Became This Family’s Worst Nightmare
josé a. alvarado jr.
Jul 3, 2024
Summary
An overwhelmed, underfunded system is jamming ERs with patients in psychiatric distress. And sometimes the consequences are deadly.
It was before dawn on May 21, 2021, just a few hours after Emily had found Andy confused, agitated and running through an orchard adjacent to her house in a rural part of the Hudson River Valley. Andy had bipolar disorder, the psychiatric condition that causes dramatic, recurring bursts of euphoric mania and deep depression, and he was in the midst of what Emily and the rest of their family had come to recognize as one of his manic phases. The 47-year-old actor/playwright was speaking rapidly and disjointedly, though with more desperation than usual. He kept talking about a searing pain he felt under his skin — the result, he said, of toxins he had absorbed while staying in a cheap hotel — and was tearing off his clothes for relief.
But Emily believed Andy could get better, because he had gotten better before. The 20-plus years since his initial diagnosis included lengthy periods when medication and counseling allowed him to laugh, love and work. In 2012, he’d gotten married to a fellow thespian; in 2013, the two had a baby girl on whom he doted. He had picked up jobs waiting tables while appearing in local Shakespeare productions and making progress toward writing plays of his own. For these stretches, Andy was on his way to realizing the potential others had seen in him ever since he was an 8-year-old starring in a production of “Pinocchio” or when he was a champion performer on the high school debate circuit.
The first step, Emily knew, was to get Andy stabilizing care at a hospital. The closest was about 20 minutes away in Kingston, the historic small city on the western banks of the Hudson, but it had closed its psychiatric wing a year before. Emily’s husband began researching options online and suggested she take Andy downriver to MidHudson Regional Hospital in Poughkeepsie. It was a larger facility that still had inpatient psychiatric beds and likely where Kingston’s emergency room would have transferred him anyway.
The drive to Poughkeepsie was hillier and about twice as long. Emily can’t remember whether Andy sat in the front or back seat, but she recalls him talking much of the way, apologizing that he was a source of such trouble for her. People experiencing psychosis frequently lack “insight,” meaning they don’t realize they are sick or experiencing symptoms, but going to the hospital had actually been Andy’s idea — a promising sign, Emily remembers thinking. At the emergency department, she gently hugged him goodbye; COVID-era rules meant she couldn’t go with him. She consoled herself that he’d get the attention he needed once the hospital admitted him and put him in a room.
But Andy never got that far.
Photographed for Huff Post, with words by Jonathan Cohn
 He Went To An Emergency Room For Help. Then He Vanished.
He Went To An Emergency Room For Help. Then He Vanished.An overwhelmed, underfunded system is jamming ERs with patients in psychiatric distress. And sometimes the consequences are deadly.
Huffpost.com
994