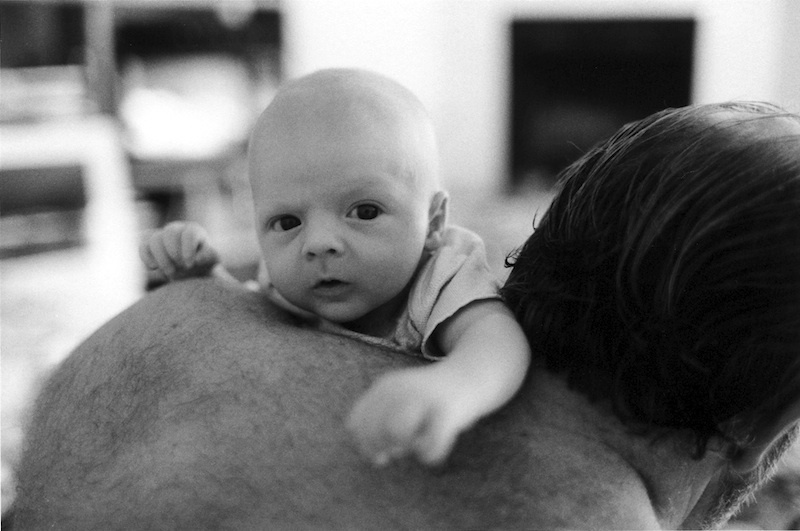
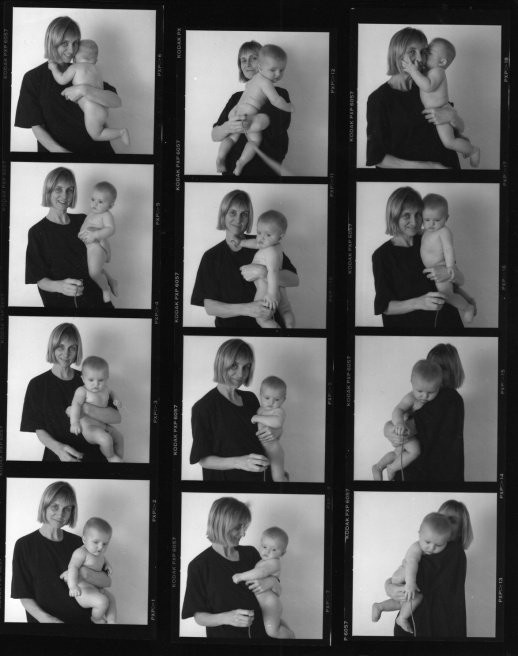
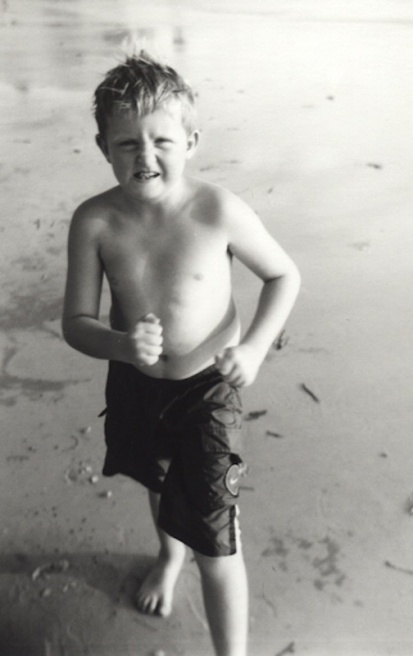
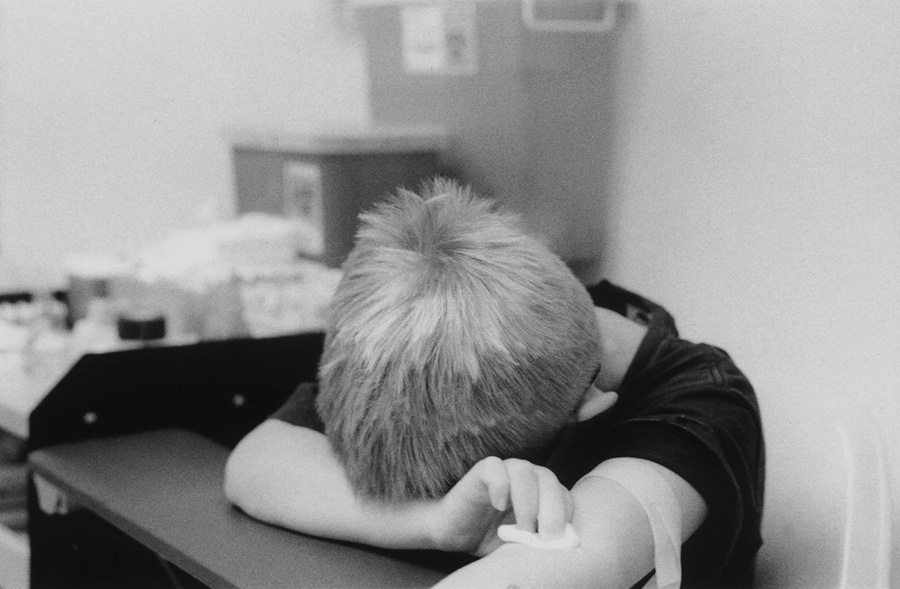
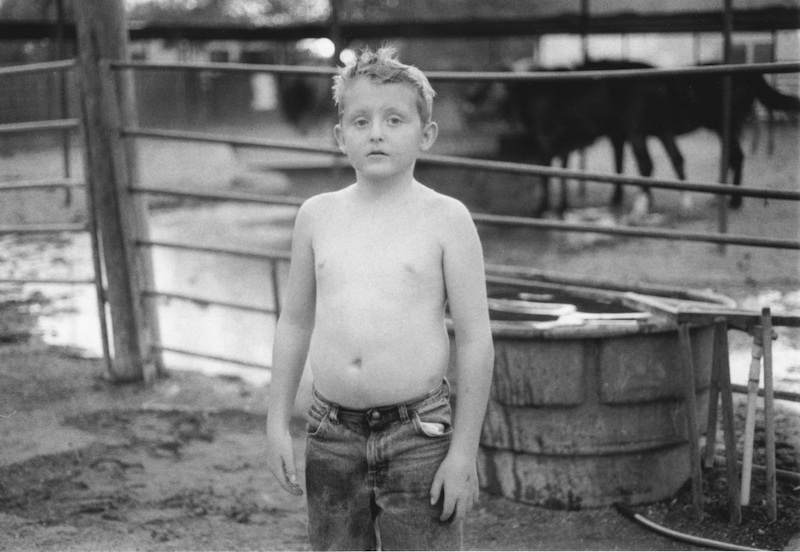
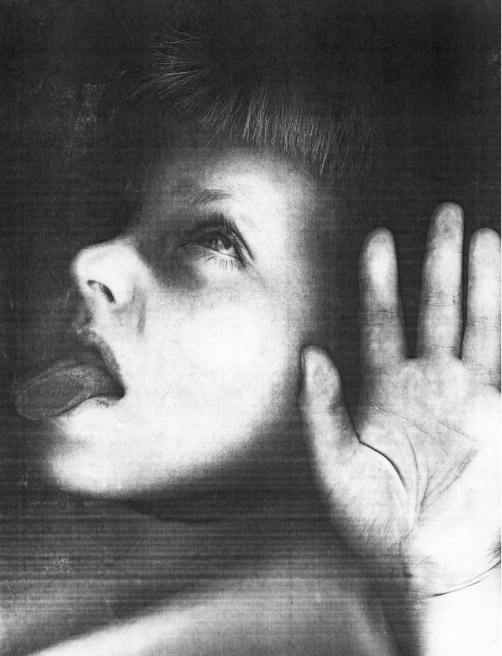
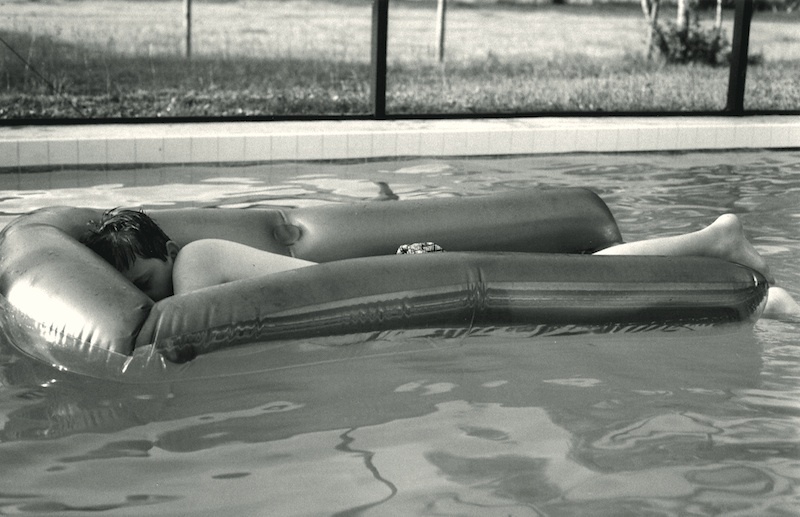
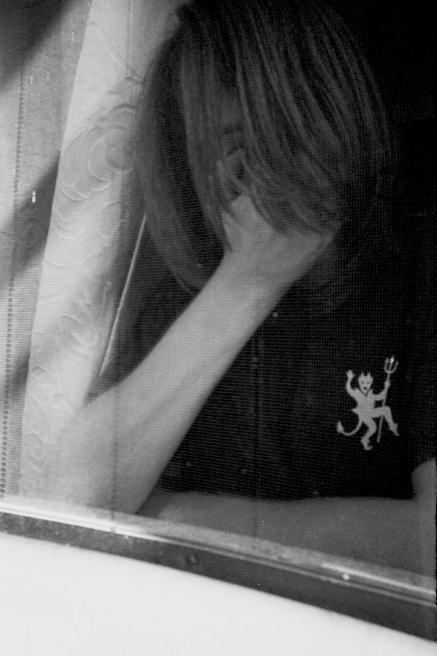
Since my son's birth, I lovingly photographed him every day to create family memories. Looking back, these images have become an extensive archive representing a mother and son's unique view of over 15 years of heartbreak, hope, sadness and terror and reveal how a family deals with their child's rapid cycling mood episodes. By sharing my story I hope parents who may be experiencing similar incidents, can detect the symptoms and get help, so that an early diagnosis can be achieved.
"My Brain is on Fire" is a fifteen year personal project about my son, who was diagnosed with Pediatric Bipolar Disorder or Juvenile Onset Bipolar Disorder, a form of bipolar disorder that occurs in children. Although, he exhibited symptoms at a very young age, he was not properly diagnosed until the age of eleven. My son showed symptoms of extreme behavior and mood changes for many years prior to being diagnosed. As a parent I sought every possible cause; parenting, nutrition, seizures, vision problems? Consistently I was told by almost every Mental Health Practitioner, "We know very little about the brain", and no one was willing or able to diagnose him sooner because childhood mental illness is a very controversial issue.
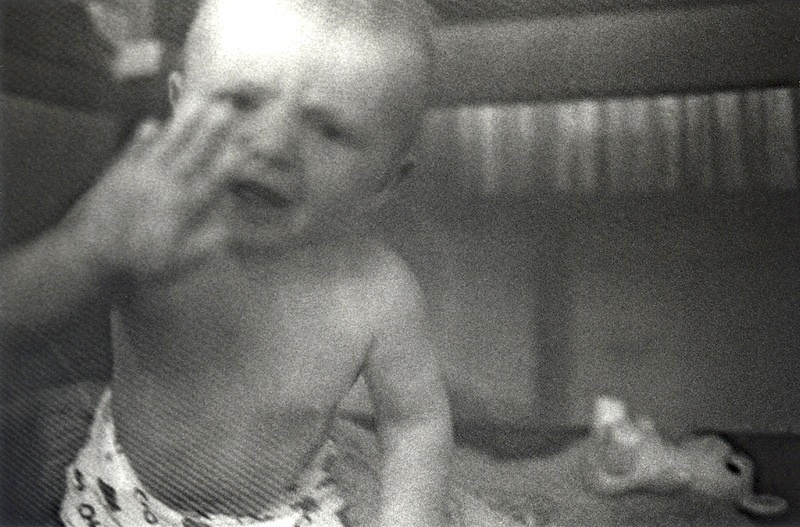
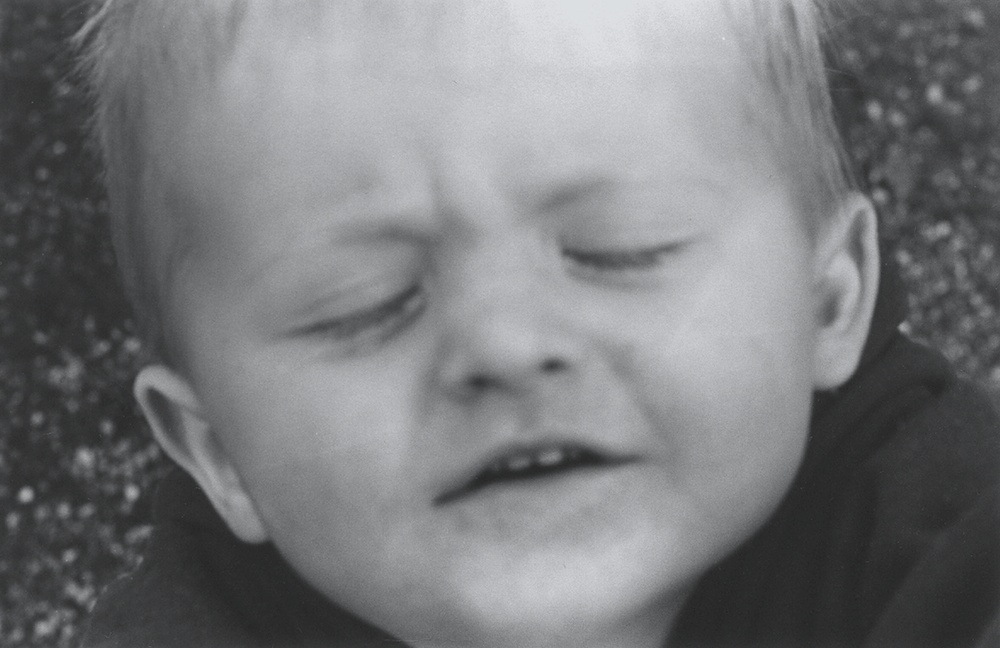
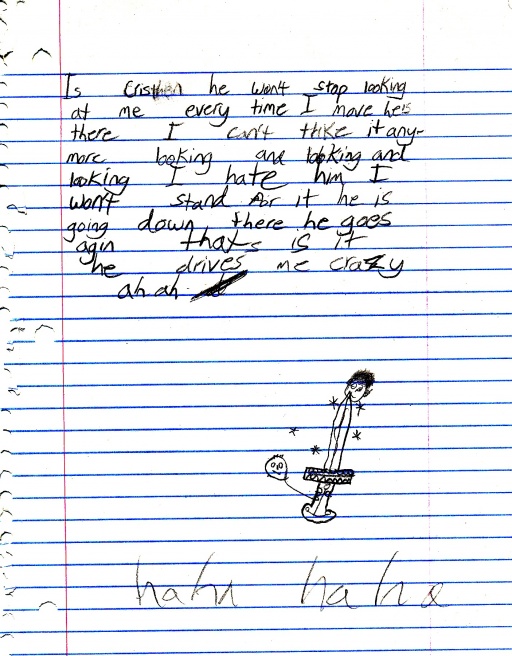
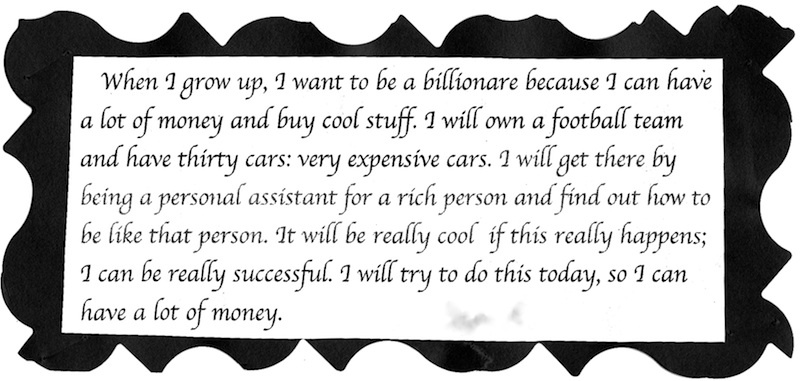
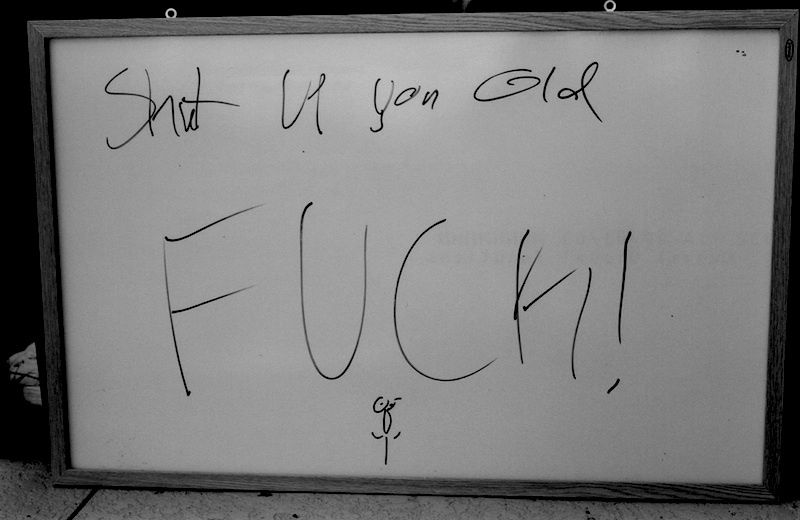
The controversy lies in the "official" diagnosis and how a child psychiatrist interprets the child's symptoms and behaviors. Even though, my son developed rages lasting over and hour within any given day and at the young age of 5 told us that he wanted to die he was diagnosed with ADHD, Oppositional Defiant Disorder and agitated depression. These are the disorders listed for children in the DSM and doctors prescribe adult psychiatric medication according to the diagnosis. My son's first psychiatric medication was an antidepressant. His mania worsened. Next amphetamines were prescribed. I refused. His brain was on fire. 6 years was spent in this vicious circle of try another drug with severe side effects never tested on children to see if it works. When he was finally diagnosed with Pediatric Bipolar Disorder by a psychiatrist we trusted he followed a treatment plan; medication and therapy, and was mainstreamed back into classes with "normal" kids. His life opened up for him, school was easier, he made friends, we had hope.
Bipolar disorders are one of several medical conditions called depressive disorders, which affect the way a person's brain functions. Depressive disorders are widespread. In the United States alone, it's estimated that more than 17.4 million adults or one of 7 people have a depressive disorder each year. Up to one-third of the 3.4 million children and adolescents with depression in the United States may actually be experiencing the early onset of bipolar disorder. (American Academy of Child and Adolescent Psychiatry, 1997) Symptoms include frequent, abrupt swings of mood and energy, intense outbursts of temper, and oppositional, defiant behaviors. The mood and behavior of children with bipolar disorder fluctuate or shift by the minute from being irritable, annoyed, and angry to a state of silly, goofy, giddiness and elation. They also enter into deep depressions: periods marked by low energy, boredom, self-recrimination and suicidal thoughts; and, suicide is the third leading cause of death among teens. Children as young as six have attempted to hang, shoot, stab or overdose themselves. The terms "early-onset", "pediatric" and "juvenile" bipolar disorder are used interchangeably as labels for a manic-depression disorder that appears early "“ very early "“ in life.
Recent studies have found that it takes an average of ten years before a child is properly diagnosed. Although many more children are now treated for mood disorders the DSM has not changed its diagnostic criteria to accommodate Pediatric Onset Bipolar disorder. In 2000 the DSM added BP-NOS (not otherwise specified) and in 2012, changed BP-NOS to NEC, (not otherwise classified). Also in 2012 a new classification for children, Disruptive Mood Disorder with Dysphoria (DMDD) was added. Neither one of these classifications support the criteria that my son exhibits and leads to preconceived assumptions and wrongful generalizations causing these children to feel ashamed and damage their already fragile self esteem.
Dr. Demetri Papolos, Director of Research of JBRF (Juvenile Bipolar Research Foundation) and co-author of the best selling book, "The Bipolar Child", has defined "The 6 Dimensions of the Fear of Harm (FOH) Phenotype" indicative of Pediatric BP illness. Dr. Papolos has given me permission to use his research criteria to caption the photographs in my photographic book and exhibition project, "My Brain is on Fire". By age 6 my son exhibited 98% of JBRF's criteria for Pediatric BP. Go to www.jbrf.org (Child Behavior Questionnaire) to learn more.
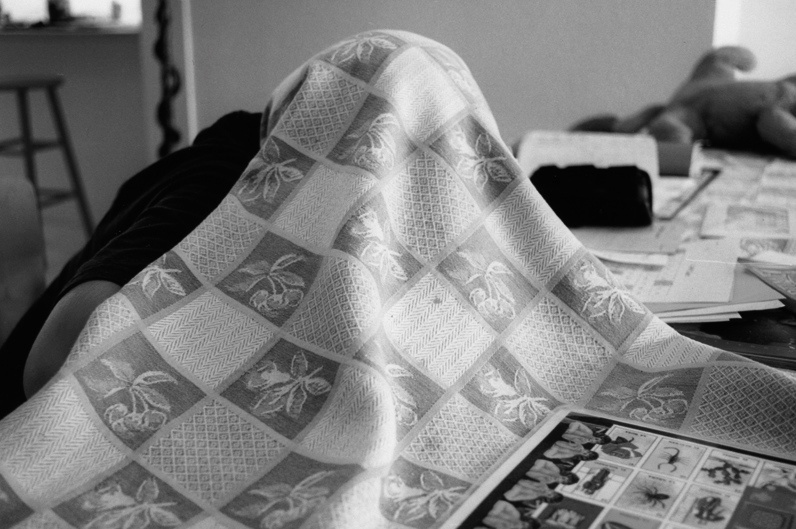
While clearly other research exists JBRF's line of research offers a very clear profile of the illness and it is the only classification with biological hypothesis. These symptoms/behaviors are best described as a fear of harm to self and others coupled with a delayed sleep phase disorder involving sleep, arousal and thermo regulation. Children with fear-of-harm experienced more severe mania and depression, more frequent hospitalizations and suffered greater school failure in terms of being held back or suspended. Research has shown that children with these symptoms are overly insulated and their body temperature fails to cool off causing anxiety and feelings of aggression. Many have a high tolerance to cold weather (not wearing a coat in sub zero weather) and over heat at bedtime which then causes sleep disturbances. The evening hours (the brain is on fire) brings frantic hyperactive behavior. Finally surrendering into sleep, they experience vivid horrific nightmares. Daybreak brings a deep, deep sleep ( sleep inertia) taking their minds and bodies hostage when they need to be awake and getting ready for school.
My son, now 21, lost his childhood to mental illness ---it is not necessary for him or anyone to lose their life due to the lack of awareness and compassion about Bipolar disorder. I believe that when more people understand this illness, there will be more resources available as well as compassion and understanding towards the families who live with this reality.
More help is needed. Offer hope, restore faith and give a young man his life. There is treatment @ John Hopkins 1000 miles away. We just need to get there. Sam has inspired me to be a better person and to understand the desperation a loved one experiences to find treatment and a correct diagnosis for mental health issues. Please go to http://gfwd.at/ZtZCgX.